Urine test strips, Medi-Test Combi 7

*taxes and shipping not included
The use of urine test strips is acknowledged as modern screening method in medical practice. Within minutes important information on the health status of the patient is obtained. This simplifies the decision about further diagnostic and therapeutic action.
| Platform | Urine test strips |
| Brand | Medi-Test |
| Parameter | Ascorbic acid, Blood, Glucose, Ketones, Nitrite, pH, Protein |
| Ascorbic acid | neg • + • ++ |
| Blood | neg • ca. 5–10 • ca. 50 • ca. 250 |
| Glucose | neg • norm • 50 • 150 • 500 • ≥1000 |
| Ketones | neg • + • ++ • +++ |
| Nitrite | neg • pos |
| pH | 5 • 6 • 7 • 8 • 9 |
| Protein | neg. • 30 • 100 • 500 |
| Selling unit | 50 Test(s), 100 Test(s) |
| Evaluable on reflectometer | No |
| Shelf life (from production) | 2 Year(s) |
| CE certified | CE-certified according to IVDR 2017/746, for professional use. |
| Remark | Optimal protection of the blood test against ascorbic acid, optimal protection of the glucose test against ascorbic acid |
| Storage temperature | 4–30 °C / 39–86 °F |
| Hazardous material | No |
The medical context of urine parameters
Urine test strips are indispensable tools in medical diagnostics to gain a rapid survey of the state of health of the patient.
Medical parameters – Principle, evaluation, sources of error, diagnosis
Albumin · Ascorbic acid (Vitamin C) · Bilirubin · Blood · Creatinine · Density · Glucose · Ketones · Leukocytes · Nitrite · pH value· Protein · Urobilinogen
Urine test strips
Albumin
Principle
The test is based on the principle of the “protein error” of indicators, i.e. at a constantly buffered pH, albumin reacts with a tetrabromophenol sulphonephthalein derivative resulting in a color change from yellow-green to green-blue.
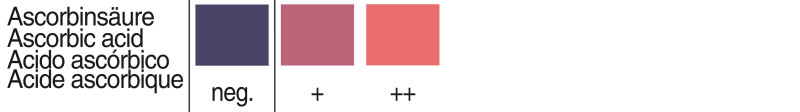
Ascorbic acid (Vitamin C)
Modern Medi‑Test urine test strips have the best available protection against influences of ascorbic acid (vitamin C) in the sample. For historic reasons, many test strips still feature a test pad for ascorbic acid.
Principle
The detection is based on the de-coloration of Tillman’s reagent. The blue colored 2,6‑dichlorophenol indophenol sodium salt is reduced to the colorless leuco form by ascorbic acid. In the presence of ascorbic acid a color change takes place from blue to red.
Evaluation
The color fields correspond to the following values:
0 (negative), 10 (+), and 20 (++) mg/dL or
0 (negative), 0.6 (+), and 1.1 (++) mmol/L.
Diagnosis
The wide spread intake of ascorbic acid (e.g. in vitamin C therapy, as a therapeutical ingredient and stabilizer of numerous medicaments, oxidation inhibitors
and preservatives in food industry) causes a rapid saturation of the organism, and a renal excretion of the excess. Interfering ascorbic acid concentrations may be reached after the ingestion of fruit juice or plenty of fruit. Therefore, the ascorbic acid test zone minimizes falsely negative results.
- High concentrations may disturb other test fields
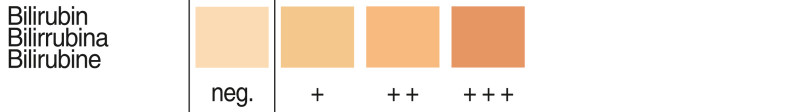
Bilirubin
Principle
A red azo compound is obtained in the presence of acid by the coupling of bilirubin with a diazonium salt.
Evaluation
The minimum sensitivity of the test strip is 0.5 to 0.75 mg bilirubin/dL urine. The color fields correspond to the following values:
0 (negative), 1 (+), 2 (++), 4 (+++) mg/dL or
0 (negative), 17 (+), 35 (++), 70 (+++) μmol/L.
Some urine components can produce a yellow coloration of the test strip. Ascorbic acid and nitrite in higher concentrations inhibit the test. Longer exposure of the urine to light leads to lowered, or falsely negative results. Higher, or falsely positive results can be caused by the presence of diagnostic or therapeutic dyes in the urine.
Diagnosis
Only conjugated (water soluble) bilirubin is excreted by the kidneys. Normally bilirubin is undetectable in urine. Bilirubinuria generally indicates liver parenchyma damage (e.g. acute virus hepatitis and other forms of hepatitis, liver cirrhosis, toxic liver cell damage) or biliary obstructions (e.g. cholangitis, obstructive jaundice).
Unconjugated bilirubin, which is detectable in serum, indicating hemolytic jaundice is not excreted by the kidneys and is absent from urine.
- Detection of liver diseases
- In combination with urobilinogendifferentiation betwaeen different forms of jaundice
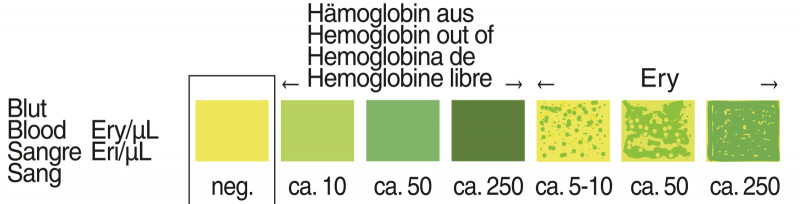
Blood
Principle
The detection is based on the pseudoperoxidative activity of hemoglobin and myoglobin, which catalyze the oxidation of an indicator by an organic hydroperoxide, producing a green color.
Evaluation
The minimum sensitivity of the test strip is 5-10 erythrocytes/μL urine corresponding to approx. 0.015 mg hemoglobin or myoglobin/dL urine. Intact erythrocytes are indicated by flecked discolourations of the test field. The color fields correspond to the following values:
0 (negative), ca. 5–10, ca. 50, ca. 250 Ery/μL, or
a hemoglobin concentration out of ca. 10, ca. 50, ca. 250 Ery/μL.
The blood test on Medi‑Test urine test strips is optimally protected against interferences by ascorbic acid. Normal concentrations of vitamin C (< 40 mg/dL) do not influence the test result. However gentisic acid still shows an inhibitory effect. Falsely positive reactions can be produced by a residue of peroxide-containing cleansing agents.
Diagnosis
Every positive reaction should be taken as a pathological finding requiring further diagnostic examinations. Hematuria (hemolysis of intact erythrocytes occurs on the test field), hemoglobinuria or myoglobinuria are frequently caused by:
Serious infections of the kidneys and urinary tract, kidney and bladder calculi, serious poisonings (e.g. benzene and aniline derivatives, chlorate, bacteria toxins, poisonous mushrooms and snake poison), heart attack, hemolysis after transfusion incident, cold hemoglobinuria or march hemoglobinuria (after strong physical exertion), different paroxysmal hemoglobinurias and serious hemolytic anemias.
- Indicator for several serious diseases
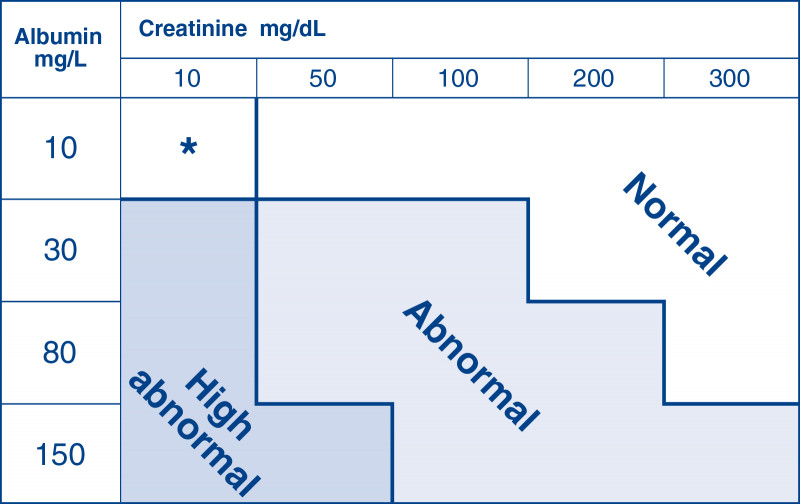
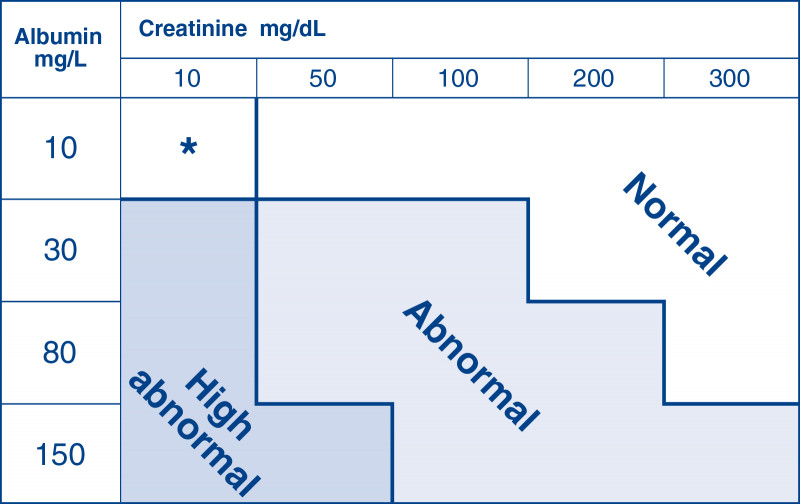
Creatinine
Principle
The detection is based on the reaction of creatinine with dinitrobenzoic acid. The resulting coloration ranges, depending on concentration, from yellow-brown to blue-black.
Evaluation
Following the determination of albumin and creatinine levels, the albumin–creatinine ratio must be ascertained, using the interpretation table printed onto the container label. This method allows use of arbitrary urine samples independent of the concentration of the urine. Thus no 24-hour urine collection is required. Using the table, the results are assigned to the urine classifications of “Normal”, “Abnormal” or “High abnormal”. The albumin-creatinine ratios classified in the table are based on the following value ranges (mg albumin/g creatinine): ¹⁾
Normal: < 30 mg/g
Abnormal: 30–299 mg/g (microalbuminuria)
High abnormal: ≥ 300 mg/g (macroalbuminuria or proteinuria)
¹⁾ Position Statement: Diabetic Nephropathy. Diabetes Care. 27. S 79-S 83 (Supplement 1), 2004
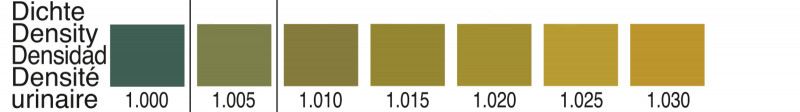
Density
Principle
The test indicates the ion concentration of urine with good correlation to the refractometric method. Increasing ion concentrations cause a color change from blue-green via green to yellow.
Evaluation
The test allows determination of the urine density between 1.000 and 1.030. The normal value for adults with normal intake of food and liquid is from about 1.015 to 1.025; however, it can vary between 1.000 after extreme liquid intake, and 1.040 after a longer period of thirst. The density measured with test strips can vary slightly from value determined with other methods, since density increases due to glucose concentrations > 1000 mg/dL (> 56 mmol/L) are not covered. Increased protein excretion can result in density values, which are too high. Alkaline urines, with high contents of buffer substances, often show results, which are too low.
Diagnosis
In kidney diagnostics determination of the urine concentration is important for checking the function of the kidney parenchyma. If high liquid intake is excluded, a very dilute urine can indicate a substantial insufficiency of the kidneys, and also a lowered ability of the kidneys to concentrate the urine, which may result from diabetes mellitus, diabetes insipidus, hyperaldosteronism or influence of diuretic drugs.
The density of the urine yields valuable supplementary information for the evaluation of other test strip parameters, and thus helps to avoid misinterpretations, especially:
during lysis of leukocytes and erythrocytes for interpreting possible differences with the sedimentation results for evaluation of the test fields for nitrite, protein and glucose
Especially in the intermediate range, between physiological and pathological results, the urine density can have a decisive role.
- Indication of the status of the kidney
- Information about the state of hydration
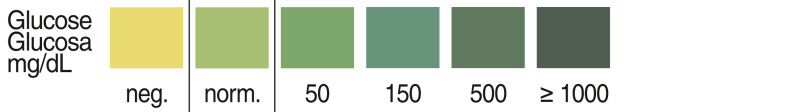
Glucose
Principle
The detection is based on the glucose oxidase-peroxidase-chromogen reaction. The oxidation of glucose by atmospheric oxygen is catalyzed by glucose oxidase to form gluconic acid lactone and hydrogen peroxide. Peroxidase catalyzes the reaction of hydrogen peroxide with the chromogen. Apart from glucose, no other compound in urine is known to give a positive reaction.
Evaluation
Pathological glucose concentrations are indicated by a color change from green to bluish green. Yellow or greenish test fields should be considered negative or normal. All test fields which have an intensity greater than the greenish negative color field must be considered positive. The color fields correspond to the following ranges of glucose concentrations:
neg. (yellow), neg. or normal (greenish), 50, 150, 500, and ≥ 1000 mg/dL or
neg. (yellow), neg. or normal (greenish), 2.8, 8.3, 27.8, and ≥ 55.5 mmol/L.
An inhibitory effect is produced by gentisic acid. Falsely positive reactions can also be produced by a residue of peroxide-containing cleansing agents. The test is not influenced by vitamin C.
Diagnosis
Because of the clear distinction between physiological and pathological glucosuria, the test is especially suitable for the detection of diabetes mellitus and for supervising (and self-supervising) of diabetes. Apart from diabetes mellitus, renal glucosuria with increased glucose concentrations may be noted during pregnancy, and after a meal with excessive carbohydrates. Every positive test reaction requires further diagnosis.
- Early detection of diabetes mellitus
- Supervision of type-II-diabetic
Ketones
Principle
The test is based on the principle of Legal’s test. Acetoacetic acid and acetone form a violet colored complex with sodium nitroprusside in alkaline medium.
Evaluation
Acetoacetic acid reacts more sensitively than acetone. Values of 5 mg/dL of acetoacetic acid or 50 mg/dL acetone are indicated. The color fields correspond to the following acetoacetic acid values:
0 (negative), 25 (+), 100 (++) and 300 (+++) mg/dL or
0 (negative), 2.5 (+), 10 (++) and 30 (+++) mmol/L
Phenylketones in higher concentrations interfere with the test, and will produce deviating colors. ß‑hydroxybutyric acid (not a ketone) is not detected. Phthalein compounds interfere by producing a red coloration.
Diagnosis
Ketone bodies including acetoacetic acid, acetone, and ß-hydroxybutyric acid are only produced in the liver. Ketones in the urine are caused by an abnormal carbohydrate metabolism. Frequently, ketonuria is a sign of diabetic ketosis, which in connection with other metabolic abnormalities may cause diabetic coma. Ketonuria may also be noted in case of insulin overdoses, starvation (e.g. slimming diet, calorie free diet), dangerous metabolic abnormalities during pregnancy (hyperemesis gravidarum), acetonemic vomiting of infants and fever caused especially by infections.
- Early detection of ketosis / acidosis
- Control-parameter for diabetes mellitus

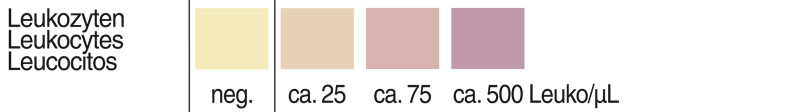
Leukocytes
Principle
The test is based on the esterase activity of granulocytes. This enzyme splits a carboxylic acid ester. The alcohol component formed during this step reacts with a diazonium salt to form a violet dye.
Evaluation
The test detects values from about 10 leukocytes/μL urine. Discolorations, which can no longer be correlated to the negative test field, and weakly violet discolorations after 120 seconds are to be considered positive. The color fields correspond to the following leukocyte concentrations:
negative (normal), 25, 75, 500 leukocytes/μL
A diminished reaction can result for protein excretion above 500 mg/dL, and a glucose concentration above 2 g/dL as well as during therapy with preparations containing cephalexin or gentamycin. Bacteria, trichomonades and erythrocytes do not give a positive reaction with this test. Formaldehyde (a preservative) can cause falsely positive reactions. Boric acid used as preservative decreases the sensitivity of the reaction.
Excretion of bilirubin, nitrofurantoin, or other strongly colored compounds can cover the reaction color. For samples from female patients vaginal secretion can simulate a falsely positive reaction. In order to avoid falsely positive results, the urine should only be sampled afterthorough cleaning of the genitals.
Diagnosis
An increased excretion of leukocytes in urine (leukocyturia) is an important symptom for infectious diseases of the kidneys and/or urinary tract (incl. the prostate).
Leukocyturia is especially important for diagnosis of chronic pyelonephritis. Often it is the only symptom between acute attacks. Other causes for leukocyturia may be: analgetic nephropathia, glomerulopathia and intoxications, cystitis, urethritis, kidney or urogenital tuberculosis, fungus and trichomonade infections, gonorrhoea, urolithiasis, tumors with obstructions.
- Symptomatic of renal and urinary tract diseases
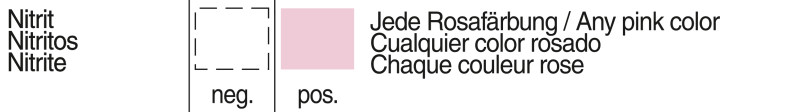
Nitrite
Principle
Microorganisms, which are able to reduce nitrate to nitrite, are indicated indirectly with this test, which is based on the principle of Griess reagent. The test paper contains an amine and a coupling component. Diazotization and subsequent coupling result in a red colored azo compound. Only nitrite can produce a diazonium salt for coupling reaction, therefore falsely positive results are virtually impossible in this case.
Evaluation
The test detects concentrations from 0.05-0.10 mg nitrite/dL urine. Any pink color indicates a bacterial infection of the urinary tract. The color intensity only shows the nitrite concentration, and does therefore not provide information about the extent of the infection. A negative result does not preclude an infection of the urinary tract, if bacteria, which cannot produce nitrite are present. Falsely negative results can be produced by high doses of ascorbic acid, by antibiotics therapy, and by very low nitrate concentrations in urine as the result of low nitrate diet or strong dilution (diuresis). Falsely positive results can be caused by the presence of diagnostic or therapeutic dyes in the urine.
Diagnosis
Bacteria, which cause infections, and can produce nitrite in the urine are e.g. E. coli (bacteria which causes most frequently infections), Aerobic Bacteria, Citrobacteria, Klebsiella, Proteus, Salmonellae and in part Enterococci, Pseudomonas and Staphylococci. If the test is positive a microscopic examination and determination of susceptibility of pathogenic bacteria to chemotherapeutic agents should follow.
- Bacterial infection of the kidneys or urinary tract
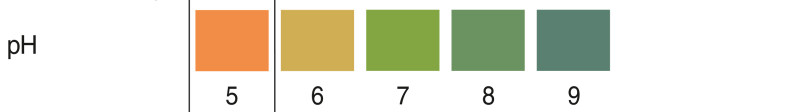
pH value
Principle
The test paper contains indicators, which clearly change color between pH 5 and pH 9 (from orange to green to turquoise).
Evaluation
The pH value of fresh urine from healthy people varies between pH 5 and pH 6. The color scale gives a clear distinction of pH value between pH 5 and pH 9. The pH should always be measured in fresh urine, since bacterial decomposition may increase the pH of the urine to values > 9.
Diagnosis
The pH value is only of significance in relation to other parameters. More acid urine (lower pH values) is found in case of an increased protein metabolism, high fever, serious diarrhoea and metabolic acidosis (serious form of diabetes mellitus). Alkalinity (increased pH value) may be noted in urinary tract infections, respiratory or metabolic alkalosis.
- Diseases of the urogenital tract
- Supplement for other parameters
- Backup for microscopic results
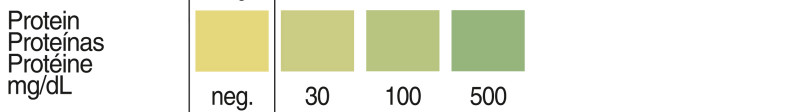
Protein
Principle
The test is based on the “protein error” principle of indicators. The test zone is buffered to a constant pH value and changes color from yellow to greenish blue in the presence of albumin. Other proteins are indicated with less sensitivity.
Evaluation
The test strip detects values above 10 mg protein/dL urine. The color fields correspond to the following ranges of albumin concentrations:
negative, 30, 100 and 500 mg/dL or negative, 0.3, 1.0, and 5.0 g/L.
Falsely positive results are possible in strongly alkaline urine samples (pH > 9), after infusions with polyvinylpyrrolidone (blood substitute), after intake of medicaments containing quinine, and also by disinfectant residues in the urine sampling vessel. The protein coloration may be masked by the presence of medical dyes (e.g. methylene blue) or beetroot pigments.
Diagnosis
The limit of a physiological proteinuria lies between 10 and 30 mg/dL. It differentiates between:
- Benign proteinuria is observed after physical strain, orthostatic proteinuria, with fever and during pregnancy. In such cases the protein excretion rate is usually normal in the first morning urine, however in the course of the day values can vary greatly.
- Extrarenal proteinuria frequently appears with acute diseases like heart insufficiency, colics, liver cirrhosis, plasmocytoma, and carcinomas.
- Renal proteinuria is caused by increased permeability of the glomerular filter and may indicate pyelonephritis, glomerulonephritis, tuberculosis of the kidneys, kidneys participation at infections and poisonings, cystic kidneys, gouty kidney. Every positive test reaction requires further diagnostic examinations.
- Symptomatic of renal and urinary tract diseases
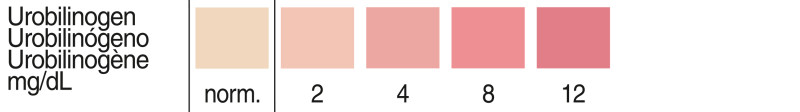
Urobilinogen
Principle
The test paper contains a stable diazonium salt producing a reddish azo compound with urobilinogen.
Evaluation
Depending on the urine color 0.5 to 1 mg urobilinogen/dL urine are indicated. 1 mg/dL is considered to be the normal excretion rate. Higher values are pathological. A complete absence of urobilinogen in the urine, which is likewise pathological, cannot be detected with the strips. The color fields correspond to the following urobilinogen concentrations:
normal (0–1), 2, 4, 8, 12 mg/dL or
normal (0–17), 34, 70, 140, 200 μmol/L.
The test is inhibited by higher concentrations of formaldehyde. Longer exposure of the urine to light leads to lowered or falsely negative results. Higher, or falsely positive results, can be caused by the presence of diagnostic or therapeutic dyes in the urine. Larger amounts of bilirubin produce a yellow coloration.
Diagnosis
An increased urobilinogen concentration in urine is a sensitive index of liver dysfunction or hemolytic diseases. Urobilinogen uria is caused by e.g. virus hepatitis, chronic hepatitis, liver cirrhosis, infections, poisonings, congestion or carcinoma of liver, hemolytic, and pernicious anemina, polycythemia and pathological state of the intestinal tract with an increased resorbence.
- Detection of liver diseases
- In combination with bilirubin differentiation between different forms of jaundice